Disinfection validation confirms that the disinfection
process eliminates or reduces harmful pathogens. Disinfectants used in the
pharmaceutical and medical device industries must be validated for their intended
use. Disinfection is a process that reduces the number of microorganisms to a
level at which they do not present a risk to patients or clients. A regulatory
expectation is to ensure the appropriate disinfectant is employed and microbial
control is maintained.
What is disinfection validation?
Disinfection Validations are used
to validate the device manufacturer's disinfection instructions. Validations may
be performed to support high-level, intermediate, and low-level disinfection
processes depending on the device's intended use. The level of
disinfection is determined by the Spaulding Category of the device, critical,
semi-critical, or non-critical.
What is the Spaulding Category
of the device?
Spaulding classification separated patient care
items into three categories critical, semi-critical, or non-critical.
Critical medical devices come in contact with the bloodstream and sterile parts
of the body. These devices must be sterilized. Semi-critical
devices come into contact with intact mucous membranes or non-intact skin but
do not normally penetrate the blood barrier or sterile area of the
patient. Semi-critical devices should be sterilized, but high-level
disinfection may be used if the device cannot withstand sterilization.
Non-critical devices only contact intact skin. Non-critical devices can
be disinfected using intermediate or low-level disinfection.
Method Outline:
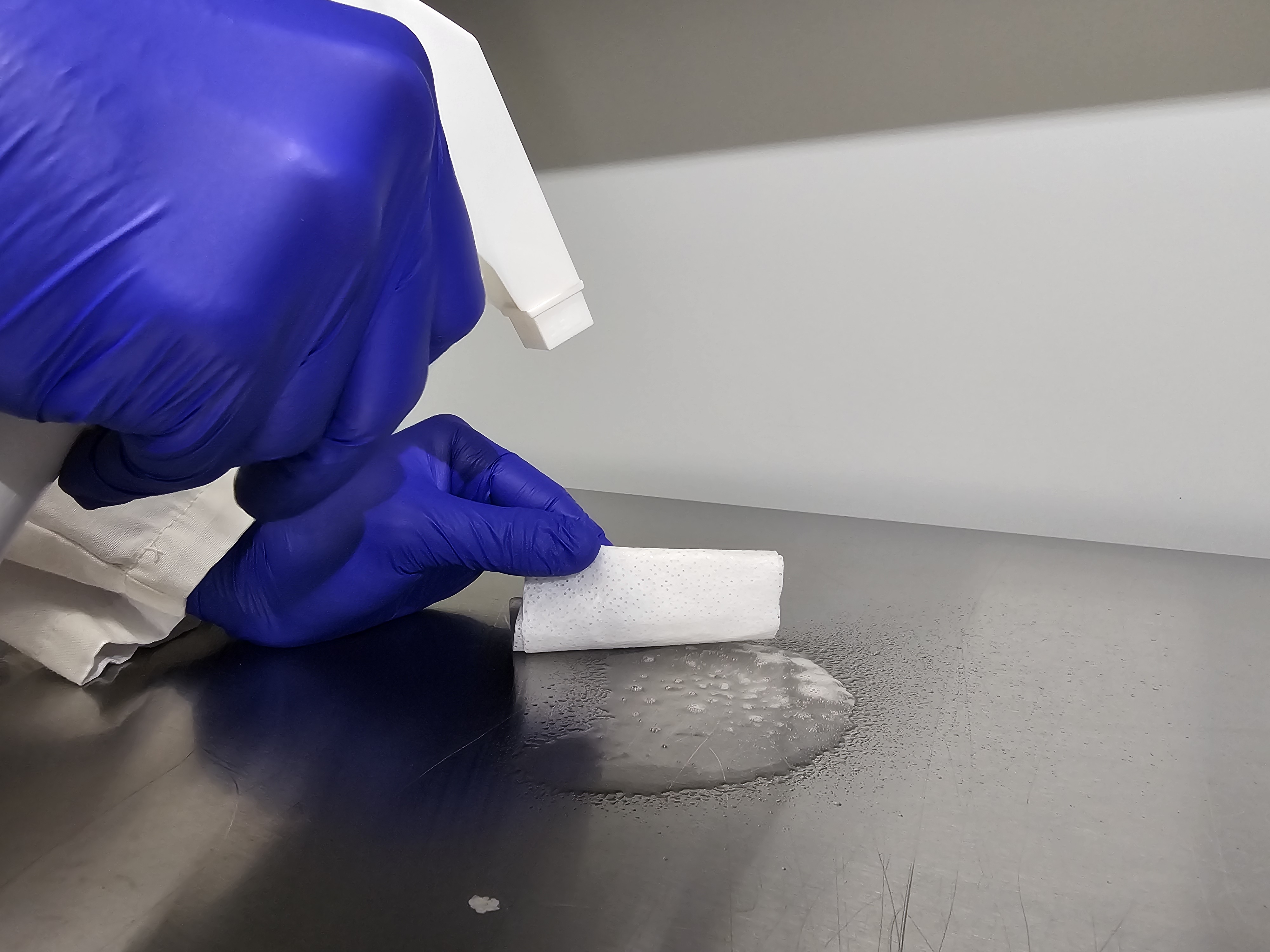
Devices are inoculated in the worst
location which is the most difficult area to clean. The sites are inoculated
with an appropriate concentration and type of microorganisms and allowed to
dry. Disinfection is performed on the inoculated test device according to disinfectant
IFU, followed by a bioburden recovery process to determine the number of
microorganisms left on the medical devices. Test devices recovery compared to a
positive control device for the log reduction.
Acceptance Criteria:
High-Level Disinfection:
• 6-log reduction of Mycobacterium spp.
Intermediate-Level Disinfection
• 6-log reduction Klebsiella pneumoniaes
• 6-log reduction Pseudomonas aeruginosa
• 6-log reduction Staphylococcus aureus
• 6-log reduction Escherichia coli
• 3-log reduction of Mycobacterium spp.
Low-Level Disinfection:
• 6-log reduction Klebsiella pneumoniae
• 6-log reduction Pseudomonas aeruginosa
• 6-log reduction Staphylococcus aureus
• 6-log reduction Escherichia coli
References:
- Food and Drug Administration 2015/(R)2017. Guidance for Industry and FDA Staff –Processing/Reprocessing Medical Devices in Health Care Settings: Validation Methods and Labeling. U.S. Department of Health and Human Services, Washington, D.C.
- AAMI TIR12:2021 Designing, testing, and labeling reusable medical devices for reprocessing in health care facilities: A guide for device manufacturers. Association for the Advancement of Medical Instrumentation, Arlington, VA.
My SteriLabs Experience as an Interdisciplinary Biochemistry and Microbiology Intern. Blog post by Natasha Tal.
September 22, 2025
Microbiologist / Study Lead (Sterilization, Sterility Testing & QMS) — 24-Month Term
September 18, 2025
Media fill testing: Ensuring Aseptic Processing for Client Projects and Licence Applications. Blog Post by Natasha Tal
August 22, 2025