Scientific advances in
diagnostics and therapeutics have led to the development of more sophisticated
medical devices. These life-changing devices vary in size, geometry,
composition, complexity, and sensitivity to cleaning, disinfecting, and
sterilizing agents.
Manufacturers of
medical devices are required under 21 CFR
801 to support product label claims by providing complete instructions for
handling, cleaning, disinfection, testing, packaging, and sterilization, as
applicable. Manufacturers also have the responsibility to conduct any testing
necessary to validate the suitability of these instructions. Moreover, it is
the manufacturer’s responsibility to consider the feasibility and ease of
cleaning the device in the intended clinical environment when designing their
device.
Why is the device design
important from the cleaning perspective?
When performing a
cleaning validation following ANSI/AAMI
ST98:2022, a worst-case use, and conditions must be simulated to represent
the highest challenge to product integrity and safety. This means that the most
difficult areas to clean have to be soiled during the study and then the least
rigorous cleaning process according to the manufacturer’s instructions has to
be applied to remove the soil from the device. If the device has a complex
geometry, hard-to-access crevices, porous surfaces, and a complex disassembly
process, there is a high chance that cleaning and consequently disinfection
and/or sterilization validation will fail, delaying regulatory clearance of the
device.
What factors to consider when
designing a new reusable medical device?
To ensure the
cleanability of a reusable medical device, several major aspects should be considered
during the design process:
1. Risk of patient infection based on intended clinical use: Be aware of the device's classification: non-critical, semi-critical
or critical, as each category will have different requirements from the
cleanability, disinfection, and/or sterilization perspective.
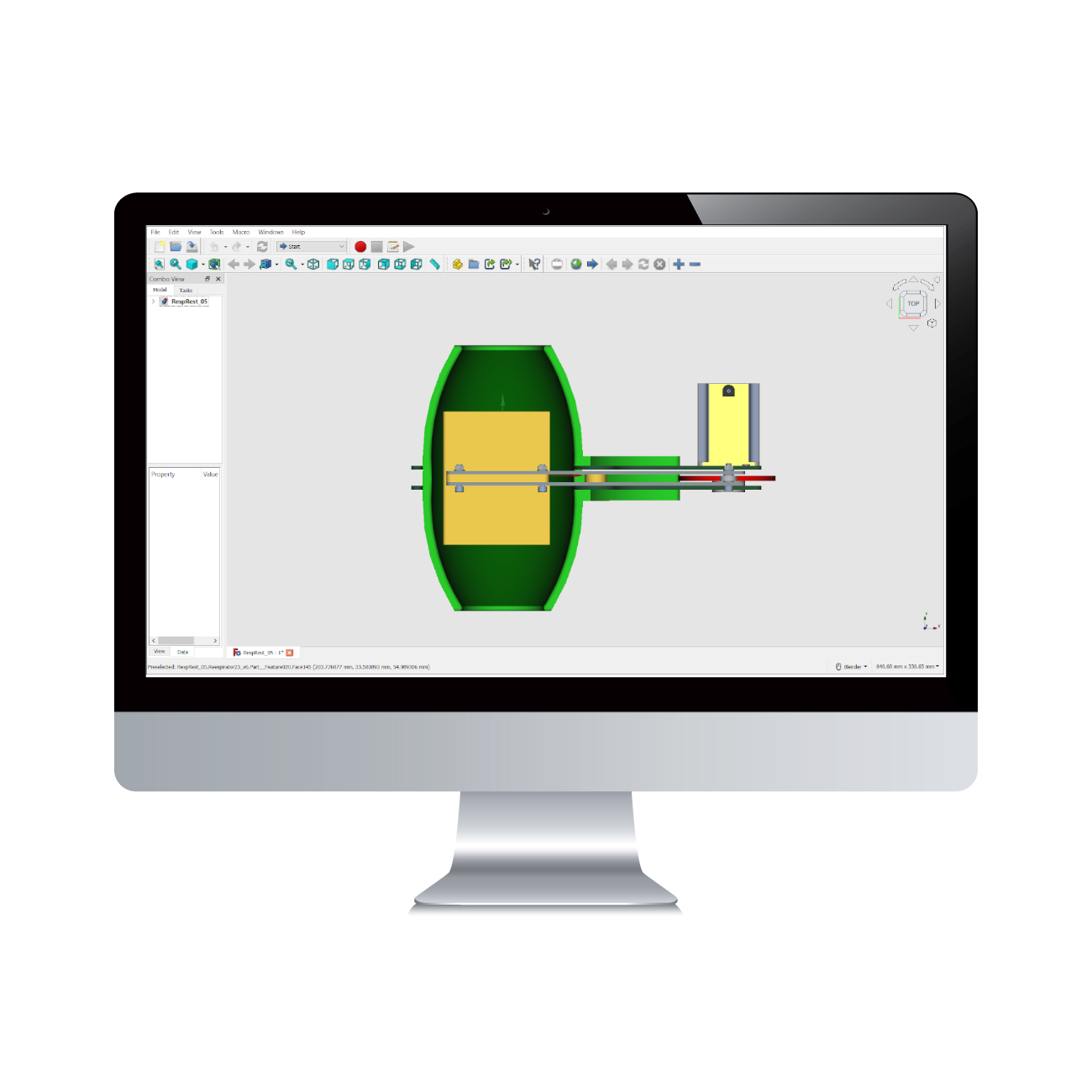
2. Physical design: Design the device with smooth, non-porous surfaces that are easy to
access and clean, while avoiding complex geometries, crevices, and corners
where contaminants can accumulate. When possible, design a fully submersible
device and isolate electronic components. If the device requires disassembly,
ensure the use of the minimum number of components, and an intuitive
reassembly.
3. Material design: Choose materials compatible with common cleaning and disinfecting
agents, and/or sterilization methods. The chosen material should withstand repeated
exposure, without degrading, corroding, discoloring, or losing structural
integrity. Some polymers, for example, offer excellent chemical resistance but
often provide limited heat resistance. In this case, alternatives such as enhancing
the material’s properties, opting for a different polymer or material, or
exploring other sterilization methods, such as ethylene oxide or hydrogen
peroxide should be considered.
4. Total system design: The impact of repeated
cleaning, disinfection, and/or sterilization on the device’s integrity and
functionality should also be evaluated. The use of screws, coating, lubricants,
and glues for example, can limit the cleaning steps, potentially causing the accumulation
of contaminants and consequently impacting the device’s service life.
If your device
incorporates complex design features, there are ways to reduce risk while
enhancing both accessibility and cleanability. Many modern devices include, for
example, ports and channels, O-rings, and articulations. For devices with
channels and ports, it's advisable to provide customized brushes as accessories
and to flush the channels. When O-rings are part of the device, it's important
to establish a routine inspection and maintenance schedule. If the device
features articulations, it should be designed to allow full actuation or
disassembly during the cleaning process.
If you need
consultation regarding the design of your new medical device with a focus on
cleaning, disinfection, and sterilization, don't hesitate to reach out to the SteriLabs’ expert team.
My SteriLabs Experience as an Interdisciplinary Biochemistry and Microbiology Intern. Blog post by Natasha Tal.
September 22, 2025
Microbiologist / Study Lead (Sterilization, Sterility Testing & QMS) — 24-Month Term
September 18, 2025
Media fill testing: Ensuring Aseptic Processing for Client Projects and Licence Applications. Blog Post by Natasha Tal
August 22, 2025